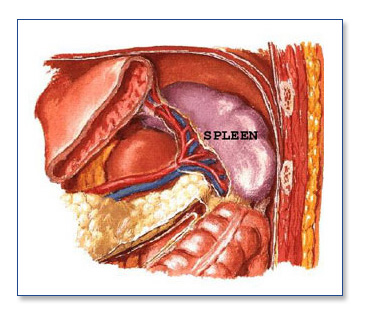
The spleen is a solid organ located in the left upper abdomen. It functions to remove old red blood cells and to assist the immune system in fighting infection. In certain diseased states, the spleen may become enlarged, inflamed, or may cause destruction of normal blood elements. One example of this is idiopathic thrombocytopenic purpura (ITP), where the spleen destroys platelets, reducing the body’s ability to clot blood. When patients fail medical therapy, they are referred for surgical removal of the spleen. Other conditions that may necessitate removal of the spleen include: hemolytic anemia, spherocytosis, thallasemia, leukemia, lymphoma, trauma, and aneurysm of the splenic artery.
Removal of the spleen (splenectomy) is usually very well tolerated once the patient recovers from the surgery. Patients require a vaccination to help prevent infection as a result of partial loss of immune function secondary to splenectomy.
Symptoms/Diagnosis
Evaluation may include blood tests, ultrasound, CT (computed tomography), angiography, or MRI of the abdomen.
Treatment
Removal of the spleen (splenectomy) is usually very well tolerated once the patient recovers from the surgery. Patients require a vaccination to help prevent infection as a result of partial loss of immune function secondary to splenectomy.
Surgery
Before and After
Your SCOSA surgeon will review with you the risks and benefits of the procedure at your clinic appointment. You will be sent for some routine lab work, X-rays, and an EKG. In addition, your SCOSA surgeon will set up any further testing required to evaluate your spleen before surgery. Occasionally an angiogram is done before the operation to block off the artery that supplies the spleen with blood. This will shrink the spleen facilitating removal.
On the day before surgery, you should have nothing to eat or drink after midnight with the exception of some medications. This will be clarified by your SCOSA surgeon. You should shower the day before or the morning of your operation.
Medications such as aspirin, coumadin, or other blood-thinning agents should be stopped at least seven days prior to surgery. Vitamin E, diet medications and St. John’s Wort should also be stopped at least one week prior to surgery. Please go over any specific questions with your SCOSA surgeon.
Patients are encouraged to stop smoking and begin an exercise program in advance of any operation.
The day of operation
Your SCOSA doctor will give you detailed instructions about where and when you should be the morning of your surgery.
Once you arrive at the hospital, a nurse will start an IV, and you will meet with your anesthesiologist and your SCOSA surgeon to answer any last-minute questions. You will likely receive some pre-operative medications and then be taken to the operating room.
After surgery, you will be in the recovery room until you are completely awake. Your room will include a breathing device called an incentive spirometer. It is important that you use this several times each hour when you are awake. The nurses on the floor will give you specific instructions about its use. In addition, it is important that you get out of bed and walk in the hall. We like our patients to do this at least once the afternoon after surgery and then at least four times each following day. These activities are vitally important to prevent a blood clot from forming in your legs, pulmonary embolism, breathing problems, and pneumonia.
After-effects of Surgery
Most patients spend one or two nights in the hospital. Some patients especially those with certain hematologic disorders will require blood or blood product transfusion around the time of the operation.
Although this operation is very safe and has a less than 1 percent mortality rate, this is an important decision for you and your physician. Potential acute complications are rare, but can include bleeding, infection, and damage to internal organs. Other less common risks are hernia, wound problems, need for open surgery or re-operation.
You should call your SCOSA surgeon immediately if you experience any of the following after this procedure: persistent fever of more than 101 degrees, persistent nausea or vomiting; worsening abdominal pain- uncontrolled by medication; increasing abdominal swelling; chest pain; shortness of breath; redness around or pus coming from incisions; or the inability to tolerate liquids.
Outcomes
The recovery period is significantly reduced from traditional surgery, and patients are typically discharged from the hospital in two to three days. Most patients return to normal activity in one to two weeks. You should follow up with your SCOSA surgeon two weeks after the operation.