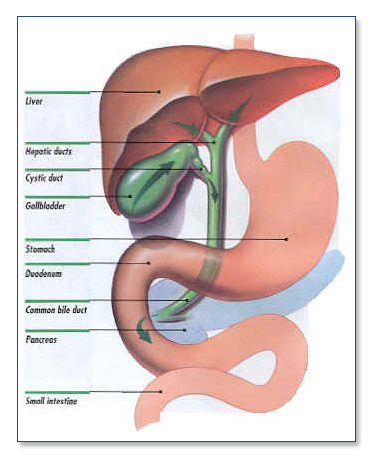
The gallbladder is a hollow organ located just under the liver. Its function is to store bile and release it when stimulated by the intake of food. Bile is used by the body help us digest our food. Sometimes the concentrations of cholesterol and bile salts in the bile lead to formation of crystals, which can become sludge or stones (calculi).
Symptoms/Causes
Stones in the gallbladder can lead to obstruction of the duct (tube) that drains the bile from the gallbladder. When food is ingested, the gallbladder contracts, trying to release bile. If the outlet is blocked with stones or sludge, patients experience pain in the right upper abdomen. This pain can be severe. It usually improves when the contraction stops.
The gallbladder can subsequently become inflamed due to prolonged obstruction. This is a condition known as cholecystitis. The pain in this situation will not let up. Another potential problem that can occur with stones is a blockage of the main bile duct. This occurs when a stone or stones get out of the gallbladder into the tubes that lead to the intestine. This can lead to jaundice (yellow skin) and severe potentially life-threatening infection. The pancreatic duct can also be obstructed at the point where it joins the main bile duct near the opening to the intestine. This can lead to inflammation in the pancreas known as pancreaitis. This, too, can be a severe life-threatening situation.
The gallbladder can also have functional problems that can cause pain. If it does not contract or empty properly (biliary dyskinesia) many of the same symptoms seen with gallstones can occur.
Treatment
Gallstones will not go away on their own, and medical (non-surgical) therapies are not successful in the management of gallstones. Surgical removal of the gallbladder is the standard of care.
You doctor can make the diagnosis in most cases with a good history and physical exam and an ultrasound of the gallbladder. If the ultrasound is normal, another study that tests the function of the gallbladder is typically done (HIDA scan with kinevac).
Once the diagnosis is made, patients are referred to a surgeon. Who should have their gallbladder removed? Anyone who has symptoms from a gallbladder problem (stones or functional), or a complication from gallstones (pancreatitis, obstruction of the common bile duct, jaundice).
Surgery
Before and After
Your SCOSA surgeon will review with you the risks and benefits of the procedure at your clinic appointment. You will be sent for some routine lab work, X-rays, and an EKG. In addition, your SCOSA surgeon will set up any further testing required to evaluate your gallbladder before surgery.
On the day before surgery, you should have nothing to eat or drink after midnight with the exception of some medications. This will be clarified by your SCOSA surgeon. You should shower the day before or the morning of your operation.
Medications such as aspirin, coumadin, or other blood-thinning agents should be stopped at least seven days prior to surgery. Vitamin E, diet medications and St. John’s Wort should also be stopped at least one week prior to surgery.
Please go over any specific questions with your SCOSA surgeon.
Patients are encouraged to stop smoking and begin an exercise program in advance of any operation. The day of operation.
The Day of Operation
Your SCOSA doctor will give you detailed instructions about where and when you should be the morning of your surgery.
Once you arrive at the hospital, a nurse will start an IV, and you will meet with your anesthesiologist and your SCOSA surgeon to answer any last-minute questions. You will likely receive some pre-operative medications and then be taken to the operating room.
After surgery, you will be in the recovery room until you are completely awake.
Depending on the severity of the gallbladder disease, you may spend time in the hospital. Patients undergoing elective outpatient gallbladder surgery almost always go home the day of the surgery.
There are different types of laparoscopic gallbladder surgery.
- Laparoscopic cholecystectomy : The gallbladder is removed using a camera and three or four tiny incisions. Today, most surgeons are able to perform this operation. Patients may return to work in about a week if the operation is performed in an elective situation. For emergency surgery, the recovery time is variable depending on the severity of the illness.
- Laparoscopic Common Bile Duct Exploration : At times, the main bile duct can be blocked by stones. These can often be removed by a gastroenterologist using a scope (ERCP). In some situations, the stones cannot be extracted, or they are detected at the initial operation done to remove the gall bladder. Most surgeons at this point would make a large incision on the abdomen and explore the common bile duct removing the stones or diverting the flow of bile. SCOSA surgeons have highly specialized training and skills and are often able to perform these procedures without making the big incision. This leads to a shorter hospital stay and recovery time.
After surgery
You should schedule a routine follow up with your SCOSA surgeon two weeks after the operation. Some patients experience a transient diarrhea after their gallbladder is removed. Although this operation is very safe and has a less than 1 percent mortality rate, this is an important decision for you and your physician. Potential acute complications are rare, but can include bleeding, infection, damage to internal organs, damage to the common bile duct or intestine, bile leak, retained stone. Other less common risks are hernia, wound problems, need for open surgery or re-operation. You should call your SCOSA surgeon immediately if you experience any of the following after this procedure: persistent fever of more than 101 degrees, persistent nausea or vomiting; worsening abdominal pain- uncontrolled by medication; increasing abdominal swelling; chest pain; shortness of breath; redness around or pus coming from incisions; or the inability to tolerate liquids.
Outcomes Most patients have complete resolution or a significant improvement of their symptoms. Typically, patients experience some soreness in the muscles of their abdomen for one or two weeks. Most patients return to work in five to seven days.