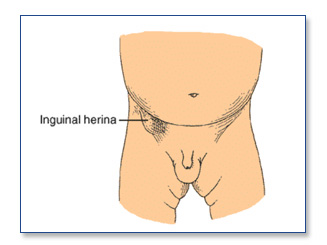
A hernia is a condition in which abdominal contents bulge through a weak area in the muscles. An inguinal hernia occurs in the groin (the area between the abdomen and thigh). It is called “inguinal,” because the intestines push through a weak spot in the inguinal canal, which is a triangle-shaped opening between layers of abdominal muscle near the groin.
Symptoms/Diagnosis
Symptoms of an inguinal hernia may include a lump or a bulge in the groin near the thigh; pain in the groin especially with lifting, coughing, or straining; pain in the testicle or cord; partial or complete blockage of the intestine.
Redness of the skin over a hernia or constant severe pain are serious findings that may suggest strangulation. This is a surgical emergency.
What Causes This? Obesity, pregnancy, heavy lifting, and straining to pass stool can cause the intestine to push against the inguinal canal. Some hernias are congenital, while others may develop over time. Hernias do not resolve without surgical correction. In fact, most hernias will enlarge over time without intervention.
Treatment
The doctor diagnoses hernia by a physical exam, X-rays, ultrasound, CT (computed tomography), and blood tests to check for blockage in the intestine.
The treatment for an inguinal hernia is surgical repair of the opening in the muscle wall. This surgery is called herniorrhaphy. The weak area is usually reinforced with mesh. This operation is called hernioplasty. If the protruding intestine becomes twisted or traps stool, part of the intestine might need to be removed.
Traditionally, these procedures have been done with a four to five inch incision in the groin. Patients are then released to normal activity in four to six weeks.
However, Laparoscopic Hernia Repair can be performed with a few tiny incisions and a camera. It is done under general anesthesia. The repair is done by placing the mesh on the inside of the strong structures in the pelvis (in contrast to most open repair). This enables patients to begin lifting almost immediately. Patients experience less pain and can return to normal activity in about two weeks.
Surgery
Before and After
Your SCOSA surgeon will review with you the risks and benefits of the procedure at your clinic appointment. You will be sent for some routine lab work, X-rays, and an EKG.
On the day before surgery, you should have nothing to eat or drink after midnight with the exception of some medications. This will be clarified by your SCOSA surgeon. You should shower the day before or the morning of your operation.
Medications such as aspirin, coumadin, or other blood-thinning agents should be stopped at least seven days prior to surgery. Vitamin E, diet medications and St. John’s Wort should also be stopped at least one week prior to surgery.
Please go over any specific questions with your SCOSA surgeon.
Patients are encouraged to stop smoking and begin an exercise program in advance of any operation.
The day of the operation
Your SCOSA doctor will give you detailed instructions about where and when you should be the morning of your surgery.
Once you arrive at the hospital, a nurse will start an IV, and you will meet with your anesthesiologist and your SCOSA surgeon to answer any last-minute questions. You will likely receive some pre-operative medications and then be taken to the operating room.
After surgery, you will be in the recovery room until you are completely awake.
Hernia surgery is usually done as an outpatient.
After-effects of Surgery
You should bring a jock strap with you to the hospital and wear it over the top of your underwear for a week or so after surgery. This will help minimize swelling. Using an ice pack in the groin area can also help with the swelling and discomfort. After the 1st 2 days, a heating pad may be helpful.
You should follow up with your SCOSA surgeon two weeks after the operation.
Although this operation is very safe and has a less than 1 percent mortality rate, complications are possible. Potential acute complications are rare but can include bleeding, infection, recurrence of hernia, damage to bowel or internal organs, damage to the vas deferens (leading to fertility problems), or damage to the blood supply to the testicle or the testicle itself can occur. It is possible that entrapment or damage of nerves in the area can lead to chronic pain or numbness. Other less common risks are incisional hernia, wound problems, need for open surgery or re-operation.
After surgery, it is common to have swelling in the cord or scrotum. Please use the jock strap and ice pack as advised. Occasionally, especially in older men, urinary retention (inability to urinate) can occur after a hernia repair. This is usually temporary for most patients, but if you absolutely can’t void after trying all of the “tricks” (ex. movement/pacing/dancing about, playing ‘waterfall-like’ sounds) – we recommend coming back to the ER where you had your surgery to have a catheter placed.
You should call your SCOSA surgeon immediately if you experience any of the following after this procedure: persistent fever of more than 101 degrees, persistent nausea or vomiting; worsening abdominal pain- uncontrolled by medication; increasing abdominal swelling; chest pain; shortness of breath; redness around or pus coming from incisions; or the inability to tolerate liquids.
Outcomes
The long-term recurrence rate for laparoscopic hernia repairs is not yet known, but the short-term results are equivalent to open repair. Currently laparoscopic repair is the preferred treatment of recurrent or bilateral hernias.